Platelet refractoriness is a significant challenge in transfusion medicine, referring to the failure of a patient to achieve the expected increase in platelet count following a platelet transfusion. This phenomenon has both immune and non-immune causes and can complicate the clinical management of patients, particularly those with hematologic malignancies or undergoing stem cell transplantation.
Causes of Platelet Refractoriness
Immune-Mediated Causes
1. Alloimmunization to HLA Class I Antigens
Human Leukocyte Antigens (HLA) are complex molecules that serve as the primary determinants for tissue compatibility in humans. Class I HLA molecules are present on almost all nucleated cells, including platelets. In the setting of platelet transfusions, the recipient's immune system can recognize these HLA antigens as foreign if they are not already present in the patient, leading to an immune response.
Mechanism of Alloimmunization
When a patient receives platelet transfusions from different donors, each transfusion episode carries a risk of introducing platelets with foreign HLA antigens. The immune system, recognizing these as non-self, can produce antibodies specific to these HLA antigens. Once alloimmunized, the recipient's plasma will contain these antibodies, which are primed to neutralize any subsequent transfusions containing platelets with the same or similar HLA antigens.
Consequence
The development of HLA antibodies leads to rapid clearance of transfused platelets from the circulation, resulting in suboptimal or negligible increases in platelet counts after transfusion. This means that even though the patient is receiving platelets, the expected improvement in clotting capability is not achieved, putting the patient at risk of bleeding complications.
Diagnostic Strategies
HLA Antibody Screening: This involves testing the patient’s serum for the presence of HLA antibodies. High-resolution assays like Luminex-based techniques can identify specific HLA antibodies, giving a more targeted approach to donor selection.
Crossmatching: Before a transfusion, the donor's platelets can be crossmatched with the recipient's serum to test for compatibility.
Management Options
HLA-Matched Platelets: The ideal strategy is to transfuse platelets that are HLA-matched to the recipient. This minimizes the risk of antibody-mediated platelet destruction.
Cross-Matched Platelets: If an exact HLA match is not available, platelets that have been cross-matched to be compatible with the recipient can also be an option, although not commonly performed.
HLA-Desensitization: In extreme cases, immunosuppressive medications or plasmapheresis can be used to reduce the levels of HLA antibodies, although these options have their own set of risks and limitations.
Challenges in Clinical Practice
Donor Pool: Finding a suitable donor is often challenging and becomes progressively harder with each transfusion episode that leads to additional alloimmunization.
Logistical Constraints: HLA-matched platelets may not always be readily available and require coordination between different blood banks and registries.
Ethnic Variability: HLA types can vary between different ethnic groups, complicating matching in ethnically diverse populations.
Cost: High-resolution HLA typing and antibody screening tests are expensive and may not be feasible in all healthcare settings.
HLA MATCHED VS HLA AVOIDANCE
HLA-Matched Platelets
Definition:
In this approach, the aim is to find a donor whose HLA antigens closely match those of the recipient. This reduces the chance of an immune response against the transfused platelets, leading to a more effective transfusion.
Methodology:
- Comprehensive HLA typing is performed for both the recipient and potential donors.
- Sophisticated matching algorithms may be used to find the closest possible match based on the HLA typing data.
Advantages:
- Lower risk of transfusion reactions and refractoriness, as the risk of antigen-antibody interaction is minimized.
- Can be highly effective in patients with known HLA antibodies, as the transfused platelets are less likely to be targeted for destruction.
Disadvantages:
- Finding a close HLA match can be time-consuming and may not always be possible, especially in ethnically diverse populations.
- More expensive due to the costs of HLA typing and the specialized handling and coordination required.
HLA Avoidance (also known as Antigen-Negative or HLA-Compatible Platelets)
Definition:
In this approach, the aim is not necessarily to match all HLA antigens between donor and recipient but to avoid those specific HLA antigens against which the recipient has developed antibodies.
Methodology:
- The recipient is tested for HLA antibodies to identify the specific antigens that should be avoided.
- Platelet units from donors lacking these particular antigens are then selected for transfusion, even if they are not a complete HLA match.
Advantages:
- Faster and often easier to implement than finding a perfect HLA match, as you only need to avoid specific antigens rather than match all of them.
- May be more readily available and cost-effective as compared to HLA-matched platelets.
Disadvantages:
- While the risk of reaction is reduced, it is not as low as with HLA-matched platelets.
- May still result in alloimmunization against other HLA antigens not previously sensitized against, as it's not a complete match.
____________________________________________________________________________________
2. Platelet-specific Alloantibodies:
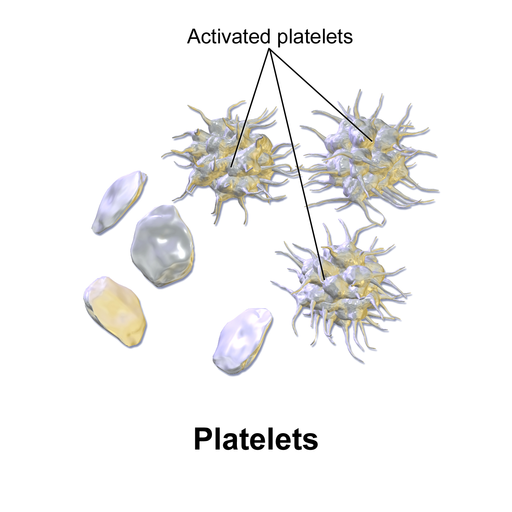
Human Platelet Antigens (HPA) are specific glycoproteins found on the membrane of platelets. Unlike HLA antigens, which are ubiquitously found on all nucleated cells, HPAs are specific to platelets. They serve as the scaffold for the binding of platelets to other cells and elements within the blood and are crucial for platelet function.
Mechanism of Alloimmunization
When a patient receives platelets from a donor with different HPAs, the recipient’s immune system can recognize these antigens as foreign and mount an antibody-mediated response against them. Like with HLA alloimmunization, the production of these antibodies is a learned response that sensitizes the immune system against future exposures to the same or similar HPAs.
Consequence
Once alloimmunized against a specific HPA, any subsequent transfusion containing platelets expressing this HPA will be targeted by the recipient's immune system. The result is rapid clearance of these transfused platelets, leading to inadequate increases in platelet count and a persistent risk of bleeding complications.
Diagnostic Strategies
HPA Antibody Screening: Similar to HLA antibody screening, this involves testing the patient’s serum for antibodies against specific HPAs. Techniques such as enzyme-linked immunosorbent assays (ELISAs) can be used for this purpose.
Platelet Crossmatching: This involves incubating donor platelets with the recipient's serum to check for compatibility, although this is more commonly done for HLA rather than HPA matching.
Management Options
HPA-Matched Platelets: These are platelets from a donor with matching or compatible HPAs to those of the recipient. Such matches are typically rarer than HLA-matches but can be highly effective in preventing refractoriness.
Immunosuppression: In extreme cases, immunosuppressive therapies may be considered to reduce antibody levels temporarily, but this comes with its own set of risks, including increased susceptibility to infections.
Challenges in Clinical Practice
Limited Awareness and Testing: HPA alloimmunization is not as well-known or as routinely tested for as HLA alloimmunization, which can result in underdiagnosis.
Donor Pool: Finding HPA-matched donors is often even more difficult than finding HLA-matched donors, particularly because routine platelet donors are not typically typed for HPAs.
Economic Considerations: Specialized tests for HPA antibodies and HPA-matched platelets can be costly and may not be available in all healthcare settings.
____________________________________________________________________________________
Non-Immune Platelet Refractory Causes
Fever and Sepsis
Mechanism: Elevated body temperature and systemic infections can lead to increased platelet consumption and turnover. In sepsis, there's often disseminated activation of the clotting cascade, which consumes platelets faster than usual.
Clinical Implication: A patient with fever or sepsis may have a lower post-transfusion platelet count increment, not because the transfused platelets are being destroyed by antibodies, but because they're being used up rapidly.
Drugs
Amphotericin B: An antifungal medication known to cause various side effects, including platelet aggregation, which might reduce the efficacy of platelet transfusion.
Heparin: An anticoagulant that can, in rare instances like heparin-induced thrombocytopenia (HIT), lead to platelet destruction.
Clinical Implication: Recognizing drug-induced thrombocytopenia is crucial, as the cessation of the offending drug can often reverse the platelet count decline.
DIC (Disseminated Intravascular Coagulation)
Mechanism: DIC is a disorder characterized by systemic activation of the blood clotting system. This leads to widespread formation of micro-clots in small blood vessels. As a result, platelets (and clotting factors) are consumed at an accelerated rate.
Clinical Implication: Patients with DIC may show poor increments in platelet counts after transfusion because of the rapid consumption of both endogenous and transfused platelets.
Splenomegaly
Mechanism: An enlarged spleen (splenomegaly) can sequester a larger portion of platelets than usual, reducing their circulating numbers.
Clinical Implication: Even after platelet transfusion, patients with significant splenomegaly might show suboptimal platelet count increments.
Graft-Versus-Host Disease (GVHD)
Mechanism: GVHD is a condition that can occur after stem cell or bone marrow transplantation, where donor cells attack the recipient's body. In the context of platelets, GVHD can contribute to bone marrow suppression, thus affecting platelet production.
Clinical Implication: Platelet refractoriness in GVHD isn't just about platelet destruction; it's also about reduced production. Addressing the underlying GVHD is crucial.
Bleeding
Mechanism: Active bleeding, especially in large amounts, can quickly consume the existing and transfused platelets.
Clinical Implication: In a bleeding patient, poor post-transfusion platelet count increments might be due to the immediate consumption of platelets at bleeding sites.
____________________________________________________________________________________
Clinical Evaluation and Diagnosis
The cornerstone of diagnosis is the calculated Corrected Count Increment (CCI) post-transfusion. A CCI lower than expected suggests refractoriness. Additional steps:
Blood Sample Analysis: To evaluate for alloantibodies against HLA and/or platelet-specific antigens.
Clinical Assessment: To rule out non-immune causes, like splenomegaly or sepsis.
_____________________________________________________________________________________
Platelet Refractory Management Strategies
Immune Mediated:
HLA-Matched Platelets: Ideally from closely HLA-matched donors or family members.
Cross-matched Platelets: Selected based on the absence of the specific antigens against which the patient has antibodies.
Desensitization: Rarely used, this involves administering the triggering antigen in increasing doses to reduce the recipient's antibody response.
Non-Immune Mediated:
Address the underlying cause, be it infection, medication, or other conditions.
____________________________________________________________________________________
Platelet Refractoriness Prevention
Leukoreduction: Removing white blood cells from transfused blood products reduces the risk of alloimmunization.
Antigen Matching: For at-risk patients, consider HLA-matched or cross-matched platelets.
Hemovigilance: For at-risk patients, transfuse platelets only when clinically indicated. If patient is not bleeding or at risk of bleeding, consider whether holding off on transfusion is possible.
____________________________________________________________________________________
Future Directions and Innovations:
Genomic Matching: Advanced molecular techniques offer potential for better donor-recipient matching.
Platelet Growth Factors: Agents like thrombopoietin mimetics can stimulate platelet production, potentially reducing the need for transfusions.
Therapeutic Modalities: Immunomodulation or extracorporeal treatments, like plasmapheresis, may play roles in specific refractory cases.