They likely want to perform a "medical splenectomy"!
Patients with ITP or idiopathic (or immune) thrombocytic purpura create an autoantibody towards antigens on platelets which subsequently marks the platelets for destruction and they are removed from circulation causing thrombocytopenia. Typically, physicians will try treatments such as steroids first, to dampen the immune systems response and see if platelet counts recover. If not, there are other options available. Very often physicians will spring for IVIg (Intravenous Immunoglobulin). The mechanism in which IVIg works in regards to platelets in ITP is not fully understood but it is postulated the immunoglobulins bind receptors on macrophages, leaving them unable to interact with platelets and target them for destruction. This inability to mark the platelets for destruction means more platelets remain in circulation.There is another option, however, and it is still considered a first-line therapy, much like IVIg is. RhIG! Yes, Rh immune globulin, the same stuff you've been giving Rh negative pregnant mothers all this time to prevent RhD alloimmunization. WinRho SDF and Rhophylac brands are approved for IV usage in ITP situations. RhoGAM (a specific brand of RhIG) is typically given only as an IM shot. RhoGAM can ultimately be used, but patients may need multiple shots, making WinRho and Rhophylac a better choice.
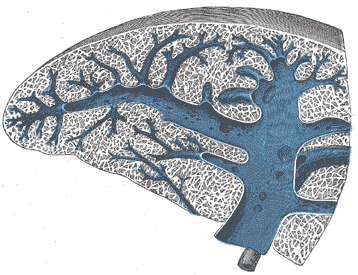
To receive IV RhIG for ITP treatment, patients MUST be Rh positive, must still have a functional spleen, and should not be exhibiting signs of hemolytic anemia or DIC. Providing RhIG to Rh positive patients for treatment of ITP is known colloquially as performing a "medical splenectomy". This is because removing the spleen is a drastic measure to stop platelet sequestration and destruction, as it is where the platelets get sent for destruction once they are antibody targeted. In more medically scientific terms it is know as an Fc receptor blockade mechanism.
This mechanism can be described as such:
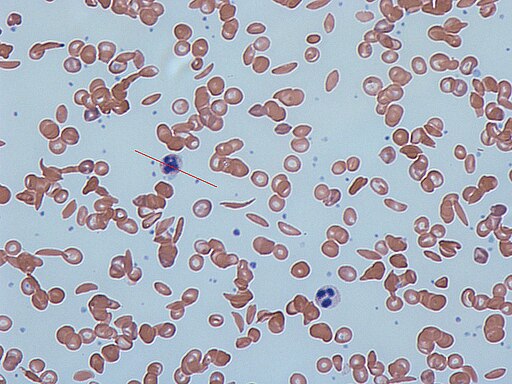
The anti-D from the RhIG preparation attaches to the RhD positive red cells of the recipient. Essentially, the RhIG "opsonizes" the RhD red blood cells, targeting them for destruction. The RhD positive red cells are brought through the reticuloendothelial system via phagocytic cells like macrophages where they will be destroyed in the spleen. This massive increase in antibody marked cells, coupled with the fact there are far more antigen sites on a Red Blood Cell, meaning more antibody can attach, means that the Red Cells will generally preferentially get removed from circulation rather than the platelets, allowing the platelets to remain in circulation.
Given this mechanism, it is not only possible, but likely that the patient can experience a level extravascular hemolysis leading to a mild decrease in Hemoglobin/Hematocrit levels. It's important to get a baseline, and continue to monitor these levels after administration. A drop of 1-2 grams of Hgb is possible over a few days post administration. This is also why it's important to ensure there aren't other hemolytic processes taking place beforehand (like hemolytic anemia). If a patients Hgb drops too much, it is thought that they should receive Rh negative blood for the time being, to lessen the amount of hemolysis taking place, ensuring the blood remains in circulation unscathed.
Despite these effects, use of RhIG is often quicker to infuse than IVIG, less volume than IVIG, sometimes longer duration of action when compared to IVIG, cheaper than IVIG, and a much more limited donor exposure than IVIG.
Have you ever seen RhIG used in such circumstances?