 |
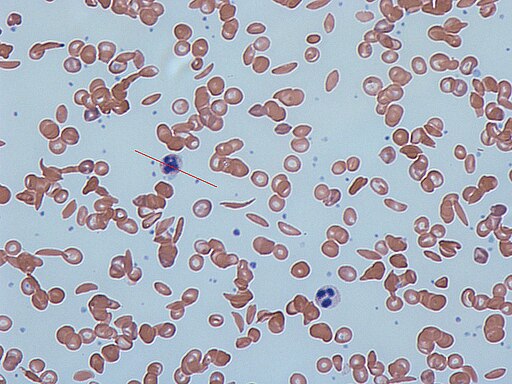
| Sickle Cells on a peripheral blood smear |
Blood Banks are no stranger to patients with Sickle Cell Anemia. Many patients are chronically transfused, and many of us have been there for emergent Red Blood Cell exchanges due to acute chest, stroke, etc. What you might not have been a part of is a Sickle Cell patient experiencing Fat Embolism Syndrome.
What is a Fat Embolism?
A fat embolism is exactly as it sounds, it's fat or globules of fat that for one reason or another enter the bloodstream circulation and act as a embolism (vasculature occlusion caused by a clot or similar). While not common, fat embolisms are usually seen in trauma with orthopedic / long bone fractures, such as tibia, fibula, femur, pelvis, etc. It can also be seen in patients with pancreatitis.
Fat Embolism Syndrome in Sickle Cell patients
Certain populations of Sickle Cell patients may be at risk for Fat Embolisms as well.
Fat Embolism Syndrome describes a situation in which Bone Marrow Necrosis occurs as a result of the patients Sickle Cell Disease. The necrosis is not fully understood but it's hypothesized that the microvasculature in the bone marrow may become occluded, leading to cell damage and death. As the Bone Marrow is necrosed, it is thought that this could lead to fat emboli being released into circulation, causing occlusion of vessels. Another theory proposes that fat globules released into circulation get broken down into toxic metabolites leading to a pro-inflammatory state, as evidenced by increased levels of CRP, cytokines, and free fatty acids in serum. These metabolites can be responsible for many of the symptoms seen in Fat Embolism Syndrome.
Patients may have shortness of breath/respiratory distress, tachycardia, neurologic changes from confusion up to coma, petechial rash, pain, fever, hepatic damage (with resulting jaundice), decreased urine output, etc.
Interestingly, patient's with more severe homozygous Sickle Cell Disease (HgbSS) are less likely to experience Fat Embolism Syndrome. Heterozygous Sickle Cell Disease such as HgbSC or HbS/ß-Thalassemia has a higher likelihood of exhibiting Fat Embolism Syndrome propensity. The thought behind this is that with heterozygous Sickle Cell Disease, patients tend to have a higher baseline hematocrit, and thus have a higher blood viscosity than that of a HgbSS patient whose hematocrits tend to trend on the lower end. This increased viscosity can lead to decreased perfusion and thus more damage, causing increased necrosis. HgbSC patients tend to have increased inflammatory issues as well, compared to their HgbSS counterparts.
Fat Embolism Syndrome Treatment with Apheresis
The Apheresis department plays a role in helping to treat Fat Embolism Syndrome. Essentially, the first line treatment of Fat Embolism Syndrome caused by Bone Marrow Necrosis in Sickle Cell Disease is to perform a Red Blood Cell exchange. This helps to remove the sickled cells that may be assisting in causing occlusions along side of the fat globules, but based on density, should also remove a portion of the fat globules as well.
Additionally, there is reason to believe that following up with a plasma exchange could be beneficial in treating Fat Embolism Syndrome. In some patients, RBC exchange is not enough. This study explores this idea. Given that there may be a biochemical component to Fat Embolism Syndrome, such as the increased inflammatory mediators, cytokines, free fatty acids, toxic lipid metabolites, etc., it makes sense that plasmapheresis would be beneficial in removing these from the plasma.
Have you come across a patient with FES?
0 comments:
Post a Comment