"I just learned about Anti-H in Bombay phenotype patients, now you're telling me there's an anti-G??"
What is Anti-G?
Anti-G is an antibody deriving relevance in pregnant or TTC (trying to conceive) prenatal women. On a normal everyday antibody screen and panel, Anti-G generally looks identical to that of a patient presenting with a combined anti-D and anti-C, in that anti-G will cause agglutination with anti-D AND anti-C positive cells. For males showing reactivity with D and C antigens, after all else has been ruled out, they will likely been resulting in their Blood Bank file as Anti-D and Anti-C. The investigation ends here.
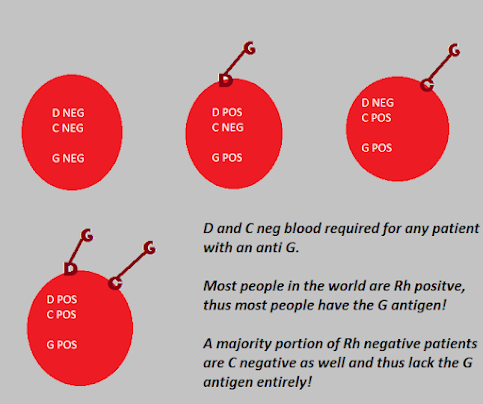
Whether it is Anti-D and Anti-C or Anti-G does not matter. The patient will receive D and C negative blood, and will thus likely have a compatible AHG crossmatch. Remember, Anti-G agglutinates with D and/or C positive blood. As long as the blood is D and C negative, they will be receiving the proper antigen negative blood regardless.
In females of childbearing age, the story is a bit different. We really want to know what is going down serologically. For a multitude of reasons. Anti-D and Anti-C can cause severe HDFN, whereas anti-G, although capable of HDFN, tends to be milder in presentation. Additionally, differentiating between Anti-D/Anti-C and Anti-G is extremely important in terms of Anti-D prophylaxis.
There are many possibilities that can take place in terms of what is really reacting when we see what looks like anti-D and anti-C reactivity on a screen/panel.
The patient could have (1) Anti-D, Anti-C, and Anti-G, (2) Anti-D and Anti-G, (3) Anti-C and Anti-G, (4) Anti-D and Anti-C, or simply (5) Anti-G. In any situation where the patient DOES NOT have an actual anti-D and is Rh negative, the patient should still follow guidelines for receiving Rh immunoglobulin at the proper intervals. Thus a patient with Anti-C and G or just anti-G is STILL A CANDIDATE for RhIG in a effort to prevent additional anti-D alloimmunization. A mother with a confirmed anti-D with or without an additional anti-G would thus not be a candidate for RhIG, allowing for the detection of any un-needed injections.
As with many transfusion centers, maternal antibodies are usually serially titered at certain intervals throughout the pregnancy as well. If a REAL anti-D or a REAL anti-C is present, it is likely that the pathologist or patient's clinicians would want to monitor the titer of these antibodies for HDFN and fetal viability purposes.
Unfortunately, most hospital blood banks do not have the capability of differentiating between AntiD/C and an Anti-G in house. The only potential clue would be if the patient had a true Anti-D and Anti-C, it's possible that a Blood Bank Technologist could potentially notice a difference in reaction strength between the two antibodies. Perhaps the anti-D is reacting at 4+ on the panel but the anti-C is only reacting at 2+. If an anti-G, it's likely that the D+ and C+ cells would react in a similar manner. This isn't concrete though, as we know.
Send Out / Immunohematology Reference Lab testing is the most common way of differentiating between these antibodies. There usually isn't any specialized testing involved...it's usually a combination of adsorptions (DOUBLE adsorptions)/elutions. It's just a very time consuming process that most hospital Blood Banks do not have the budgeted FTEs for.
Check out these links for more info on lab testing that differentiates between G and D/C
0 comments:
Post a Comment